common gut issues in babies and how to manage them
Written by Emily Else
You’ve read the books, done the antenatal classes, and entered a whole new world of caring for your baby. You may not however, be prepared for what follows if your baby suffers with gastrointestinal symptoms. You may ask yourself ‘what is normal?’, ‘when should I be concerned?’, ‘does my baby have an intolerance?’. You are certainly not alone in asking these questions, as a Paediatric Dietitian I hear these on a daily basis.
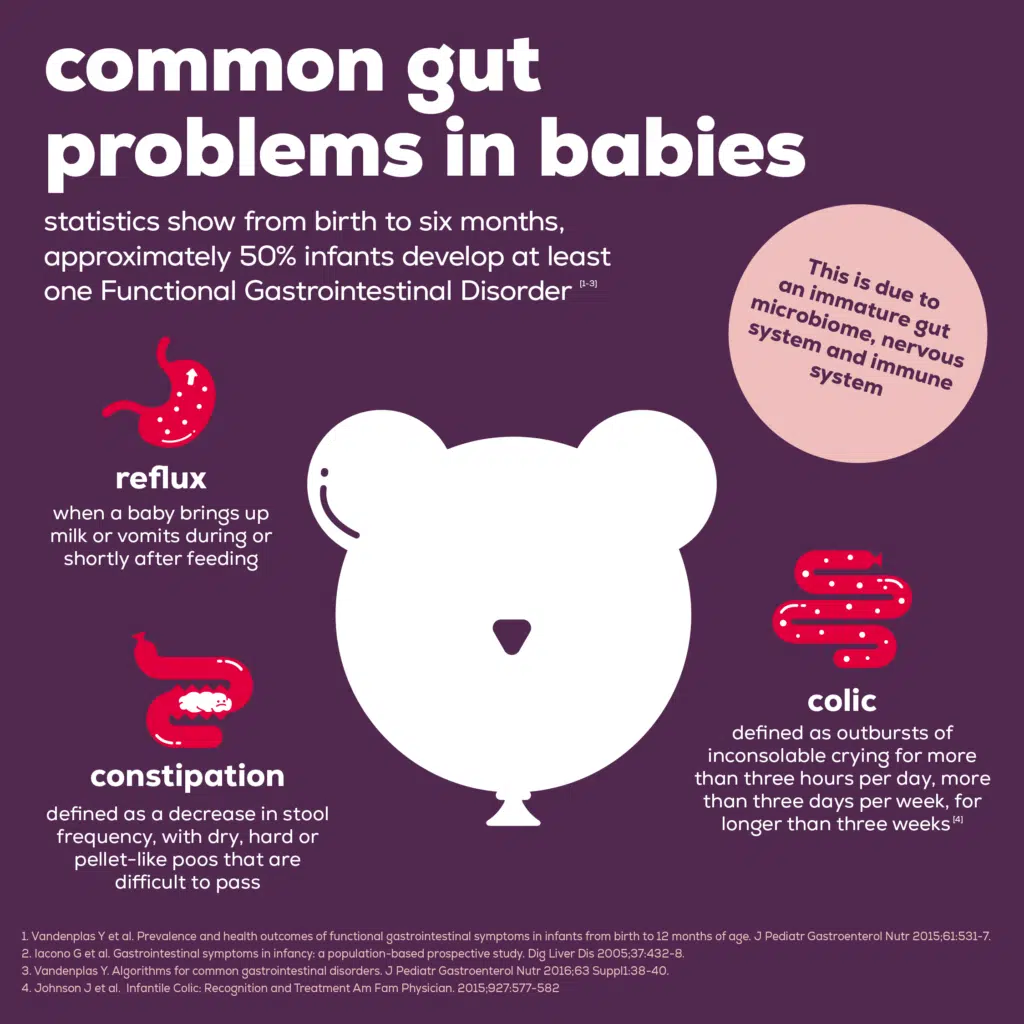
During the first six months of life, it is common for babies to experience a range of gastrointestinal symptoms. Following a consultation with your GP, often there is no obvious medical cause. The term for this collection of symptoms is Functional Gastrointestinal Disorders (FGIDs).
Statistics show from birth to six months, approximately 50% of infants develop at least one FGID [1-3]. This is due to an immature gut microbiome, nervous system and immune system. The most common FGIDs are reflux (affecting 30% of infants), colic (affecting 20% of infants) and constipation (affecting 15% of infants) [1]. It is not uncommon for infants to experience more than one FGID.
Symptoms usually improve spontaneously within the first year of life, nevertheless this period of time can be distressing leading to a cascade of worry, sleepless nights, multiple GP visits, reduced breastfeeding… not to mention the late night google searches, amazon buys and social media scrolling in search of the magic answers!
This article discusses the most common FGIDs and how to manage them.
Reflux
Reflux is when a baby brings up milk or vomits during or shortly after feeding. The muscle at the top of the stomach is immature early in life, resulting in milk passing back up the oesophagus, especially when lying down. This can be uncomfortable for babies resulting in screaming and back arching. Reflux usually starts before a baby is 8 weeks old and resolves by 1 year of age [4].
How to improve your baby’s reflux symptoms:
- Seek advice on positioning during feeds from a health visitor or breastfeeding specialist
- Try to feed your baby in an upright position if comfortable and keep baby upright for 30 minutes after a feed
- Wind in the middle of the feed as well as at the end
- If formula feeding, ensure your baby is not drinking excessive volumes, use the guide on the tin and seek advice if unsure
- A thickening agent may be prescribed before breastfeeds or if formula feeding anti-reflux formula is available which has a thickened consistency. This helps the milk stay down in the stomach [4-5]
Colic
Colic is defined as outbursts of inconsolable crying for more than three hours per day, more than three days per week, for longer than three weeks [6]. The crying usually peaks at 6 weeks of age and resolves by 4-6 months of age [7]. The exact cause of colic is unknown but one hypothesis is due to babies have difficulty digesting food when they are young.
How to improve your baby’s colic symptoms:
- Position your baby as upright as possible during feeds to prevent them swallowing air
- Wind your baby after each feed
- Comfort your baby by rocking, singing, holding, swaddling
- Try a warm bath
- Try white noise as a distraction when they are crying
- Get support for yourself if feeling overwhelmed, share the care if possible
- You may have heard about anti-colic drops, gripe water, herbal remedies, probiotics and changes to your diet if breastfeeding but there is very little scientific evidence that these work [1,8]
Constipation
Constipation is defined as a decrease in stool frequency, with dry, hard or pellet-like poos that are difficult to pass. Most babies will poo four times per day in the first week of life, with a reduction to two per day at 1 year of age [9]. Constipation can occur if your baby becomes dehydrated due to illness or teething and sometimes following the introduction of formula milk or weaning foods which are harder to digest than breastmilk.
How to improve your baby’s reflux symptoms:
- Offer frequent breastfeeds
- If formula feeding, ensure preparation of the milk follows the manufacturer’s instructions
- If formula feeding, try offering extra water between feeds
- If your baby has started solids, try including fruits like apple, pear and prune and sips of water with meals
- Bicycle legs – moving legs in a bicycle motion and tummy massage may help to stimulate the bowels
- If these have not helped within 1-2 weeks, prescription medication may be available
Could reflux, colic or constipation be linked to lactose intolerance or cow’s milk allergy?
Lactose intolerance is a digestive problem where the body is unable to digest lactose, a sugar found in milk. This is rare in babies and is most likely to occur temporarily after a bout of gastroenteritis. Symptoms include watery diarrhoea, wind and tummy cramps.
Cow’s milk allergy occurs when the immune system reacts to the proteins found in milk. It is more common than lactose intolerance, estimated to affect up to 7% of babies under 1 year [10]. Reflux, colic and constipation are all digestive symptoms of cow’s milk allergy. Your GP may consider a milk-free diet trial if the above suggestions have not worked. For breastfed babies, treatment involves the mother following a milk-free diet and if formula fed, a hypoallergenic formula is prescribed [11].
When to seek further advice
For the majority of babies, the above steps can help and symptoms will improve as their guts mature. It is important to speak to your GP if none of the above approaches help, you are struggling to cope with their symptoms or you experience new worrying symptoms such as vomiting, blood in their poo or baby is not gaining weight.
References
- Vandenplas Y et al. Prevalence and health outcomes of functional gastrointestinal symptoms in infants from birth to 12 months of age. J Pediatr Gastroenterol Nutr 2015;61:531-7.
- Iacono G et al. Gastrointestinal symptoms in infancy: a population-based prospective study. Dig Liver Dis 2005;37:432-8.
- Vandenplas Y. Algorithms for common gastrointestinal disorders. J Pediatr Gastroenterol Nutr 2016;63 Suppl1:38-40.
- National Institute for health and care excellence. Gastro-oesophageal reflux disease in children and young people: diagnosis and management. London: NICE; 2015. Available at: https://www.nice.org.uk/guidance/ng1/resources/gastrooesophageal-reflux-disease-in-children-and-young-people-diagnosis-and-management-pdf-51035086789[Accessed July 2022]
- Salvatore S et al. Review shows that parental reassurance and nutritional advice help to optimise the management of functional gastrointestinal disorders in infants. Acta Paediatr 2018; doi:10.1111/apa.14378.
- Johnson J et al. Infantile Colic: Recognition and Treatment Am Fam Physician. 2015;927:577-582
- National Institute for health and care excellence. Colic, infantile. London: NICE; 2017. https://cks.nice.org.uk/colic-infantile[Accessed July 2022]
- Vandenplas Y et al. Functional Gastrointestinal Disorders in Infancy: Impact on the Health of the Infant and Family. Pediatr Gastroenterol Hepatol Nutr. 2019; 22(3):207-216
- National Institute for health and care excellence. Constipation in children and young people: diagnosis and management. London: NICE; 2010. https://www.nice.org.uk/guidance/cg99[Accessed July 2022]
- NHS Choices. Cow’s Milk Allergy. Available at https://www.nhs.uk/common-health-questions/childrens-health/what-should-i-do-if-i-think-my-baby-is-allergic-or-intolerant-to-cows-milk [Accessed July 2022]
- National Institute for health and care excellence. Cows Milk Allergy in Children. London: NICE; 2021. https://cks.nice.org.uk/topics/cows-milk-allergy-in-children [Accessed July 2022]
About the author
Written by Emily Else BSc Hons Specialist Paediatric Dietitian at City Dietitians.
Emily is a registered dietitian specialising in infant and child nutrition. She advises on a range of nutritional concerns including digestive issues and food allergy.