IBS and The Gut Brain Axis
Written by Annabel Sparrow ANutr
Brought to you by 
What is IBS?
Unsurprisingly, many of you may have heard of irritable bowel syndrome or IBS for short, as it is thought to affect about 1 in 10 of us in the UK (1), that’s A LOT when you think about it! But, do you know what it actually is, how it’s linked to your brain (yup) and how you can manage it? We’ve gut you covered …
Cramps, bloating and GI discomfort, sound familiar? These are just a few of the symptoms that can accompany IBS … but did you know there are four different types of IBS? Each with their own unique set of symptoms. We’ll cover all four later on, but before we dive in, what actually is IBS and what causes it?
Many of us come to hear of IBS due to the gastrointestinal symptoms, however it is now known as a disorder of gut-brain interaction, specifically when the communication pathway between the two becomes disrupted. Psychological symptoms, such as stress, anxiety and depression are common in IBS, and many play a role not only in the exacerbation of IBS, but also the development … SO much so that IBS was re-defined as a disorder of the gut-brain axis (2), more on this to come …
Firstly, why does this happen? Sadly it’s not a simple cause and effect, there are a variety of reasons why people may develop IBS, and it’s unlikely that there is just one single cause. Research suggest some factors which contribute to IBS may include:
- Imbalances in gut microbes
- Gastrointestinal infections/gastroenteritis
- Changes to gut barrier function
- Low-grade inflammation
- Pain hypersensitivity in organs like the stomach and intestines
- Long term use of certain medications such as antibiotics
There is also often an overlap in people with IBS and people with food intolerances, certain vitamin deficiencies, and small intestinal bacterial overgrowth (SIBO) (17).
The Gut Brain Axis and IBS
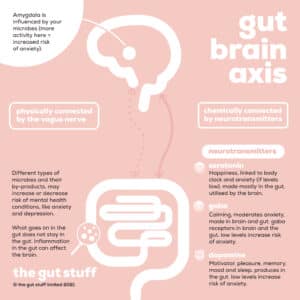
Now we know IBS is classified as a disorder of the gut-brain axis – what actually is the gut-brain axis?
As you can see, there is a communication system between your gut and brain. This connection is bi-directional – think of it as two pals keeping each other company and feeding off each other’s vibe. Chatting physically via the vagus nerve (aka the telephone wire) and chemically through hormones called neurotransmitters (aka whatsapp). This nerve is pretty remarkable and plays a key role in our body, including breathing, our heart rate, digestion and even our immune response. It’s also a key player in our parasympathetic nervous system (our ‘rest and digest’ control centre), which, when activated, has a knock-on effect of settling our sympathetic nervous system (our ‘fight or flight’ control centre).
Pretty clever stuff! There’s a lot of cross-talk going on, what goes on in your gut is going to have an effect on your brain and vice versa.
To put this into context, a lack of microbial diversity and even specific species have been linked with poor mental health. Interestingly, studies have shown that imbalances in the gut microbiome are associated with IBS (5,6). Why is this important? The gut bugs also produce neurotransmitters e.g. cortisol, the stress hormone, and serotonin (most of our serotonin is made in the gut). They also stimulate immune cells to produce cytokines which deliver messages to the brain (18).
The gut-brain axis, maybe unsurprisingly, has been linked to many diseases and disorders, not just IBS (3), but also depression and anxiety (4) amongst others.
In summary, it’s not just our diet affecting our gut health, our brain has a big impact on our gut too. Therefore, when approaching managing your symptoms, a multifaceted approach is worth considering. Sceptical? We get it, however research is now showing non-dietary approaches that target the gut-brain axis (e.g. cognitive behavioural therapy, relaxation techniques, and yoga) could be equally as effective in improving IBS symptoms as dietary interventions (16). The results will differ from person to person, however it is definitely food for thought if you suffer with IBS!
Symptoms
Symptoms of IBS vary from individual to individual and in severity. These include tummy pain, related to pooing (i.e. the pain is often associated with a change in how often you poo), or the consistency of your poo, such as diarrhoea or constipation. Bloating is also really common in IBS, although not a diagnostic criteria.
There are four types of IBS, based on the type of poo you typically have on a ‘bad’ day:
IBS D – Diarrhoea Predominant
IBS C – Constipation Predominant
IBS M – Mixed (both diarrhoea and constipation)
IBS U – Unclassified (you may experience a mix of symptoms which may change over time)
However, people can also experience bloating, farting, passing mucus from the bottom, tiredness and lack of energy, feeling sick, backache and bowel incontinence. As well as this IBS can have a serious impact on people’s daily lives and quality of life (10,14).
Managing IBS
Now you know the facts, there are steps you can take to help manage your symptoms, which can have a huge difference in reducing unpleasant symptoms, regardless of your IBS type.
There are plenty of lifestyle changes you can consider to help manage your symptoms:
- Movement: walking and stretching, as well as twists and breathwork in yoga can be effective.
- Sleep: is when your body rests and rebuilds so quality sleep is important.
- Stress management: stress is known to exacerbate symptoms, therefore stress management techniques such as breathwork, mindfulness, yoga, journaling or talking to a loved one could be helpful.
- Clothing: avoid tight waistbands which can lead to uncomfortable bloating especially around meals.
- Peppermint oil capsules: can be effective for some in easing bloating or cramping.
- Mindful eating: not just what you eat but how – avoid eating in front of screens, and remember to chew, chew and chew again!
- Diet: some food can trigger or worsen symptoms, if you find this it’s best to work with a healthcare professional to safely manage this.
- Probiotics: new evidence suggests certain strains of probiotics may help to alleviate symptoms of IBS, however the dose and specific bacterial strain are important (15), so make sure you read up first. The powers that be (aka the European Food Safety Authority ESFA) have also said that findings from IBS studies can be applied to people without IBS who experience occasional gut discomfort.
The effectiveness of the above will vary from person to person, so try them out and find out what works best for you.
Want to learn more about your symptoms, and what you can do about them? Download the gut stuff app for free, to read more and speak to gut experts for less.
This article is sponsored by PrecisionBiotics, find out more information here.
References:
Black,C.J., Ford,A.C., (2020) “Global burden of irritable bowel syndrome: trends, predictions and risk factors.” Nat Rev Gastroenterol Hepatol. 17(8). doi: 10.1038/s41575-020-0286-8.
International Foundation for Functional Gastrointestinal Disorders. https://aboutibs.org/what-is-ibs/psychological-factors-and-ibs/. Accessed 06.01.22 2. Schmulson and Drossman. 2017;23(2):151-163
3.Irritable bowel syndrome: A microbiome-gut-brain axis disorder?”, World Journal of Gastroenterology, 20(39), p. 14105. doi: 10.3748/wjg.v20.i39.14105.
4.Liu, L. and Zhu, G. (2018) “Gut–Brain Axis and Mood Disorder”, Frontiers in Psychiatry, 9. doi: 10.3389/fpsyt.2018.00223.
Wang,L. Et al., (2020) “Gut Microbial Dysbiosis in the Irritable Bowel Syndrome: A Systematic Review and Meta-Analysis of Case-Control Studies.”, J Acad Nutr Diet. doi: 10.1016/j.jand.2019.05.015.
Zhang,T., et al., (2022) “Efficacy of Probiotics for Irritable Bowel Syndrome: A Systematic Review and Network Meta-Analysis.”, Front. Cell. Infect. Microbiol., 12. doi.org/10.3389/fcimb.2022.859967
Mukhtar et al., (2019) “Functional gastrointestinal disorders and gut-brain axis: What does the future hold?”. World J Gastroenterol. 25(5). doi: 10.3748/wjg.v25.i5.552.
A major organ plays an unprecedented role in choosing what you eat (2020). Available at: https://www.inverse.com/mind-body/gut-brain-axis-controls-food-choice (Accessed: 29 June 2020).
Irritable Bowel Syndrome. https://www.nhs.uk/conditions/irritable-bowel-syndrome-ibs/symptoms/. Accessed 20.03.24. NHS, 2021.
Canavan,C., West,J., Card,T., (2014) “Review article: the economic impact of the irritable bowel syndrome.”, Aliment Pharmecol Ther., 40 (9). doi: 10.1111/apt.12938.
Black,C.J., Ford,A.C., (2020) “Global burden of irritable bowel syndrome: trends, predictions and risk factors.” Nat Res Gastroenterol Hepatol., 17 (8). doi: 10.1038/s41575-020-0286-8.
Dean et al., (2005) “Impairment in work productivity and health-related quality of life in patients with IBS”. Am J Manag Care., 11 (1).
Gralnek et al., (2000) “The impact of irritable bowel syndrome on health-related quality of life.” Gastroenterology. 119 (3).doi: 10.1053/gast.2000.16484.
Frank et al., (2002) “Health-related quality of life associated with irritable bowel syndrome: Comparison with other chronic diseases.” Clinical Therapeutics. 24 (4). Doi: 10.1016/S0149-2918(02)85143-8.
Irritable bowel syndrome in adults: diagnosis and management. https://www.nice.org.uk/guidance/cg61/chapter/Introduction. Accessed 20.03.24. National Institute for Health and Care Excellence. Online. 2008.
Biesiekierski,J,R. Et al., 2022. “Review article: exclude or expose? The paradox of conceptually opposite treatments for irritable bowel syndrome.” Aliment Pharmacol Ther. doi: 10.1111/apt.17111.
Vasant DH, Paine PA, Black CJ, et al. British Society of Gastroenterology guidelines on the management of irritable bowel syndrome. Gut. 2021;70(7):1214-1240.
Cryan JF, O’Riordan KJ, Cowan CSM, et al. The Microbiota-Gut-Brain Axis. Physiological Reviews. 2019;99(4):1877-2013.
Schmulson MJ, Drossman DA. What Is New in Rome IV. Journal of Neurogastroenterology and Motility. 2017;23(2):151-163.