allergies
Written by Dr. Jenna Macciochi
Ask your grandparents. It’s likely that when they were children, they had probably never heard of anyone being allergic to milk or to peanuts. In fact, before the 1990s, peanut allergies were so rare that barely any data on them were collected (1). And what about now? One can bet for sure you know people who have (or claim to have) an allergy.
It’s clear that the incidence of allergies is now steeply climbing, showing no signs of abating. Worryingly, the UK has among the highest prevalence in Europe with over 20% of the UK population affected by one or more allergic disorders (2, 3). This brings with it a daily fear of a possible asthma attack, the persistent uncomfortable itch to anaphylactic shock from an allergic reaction.
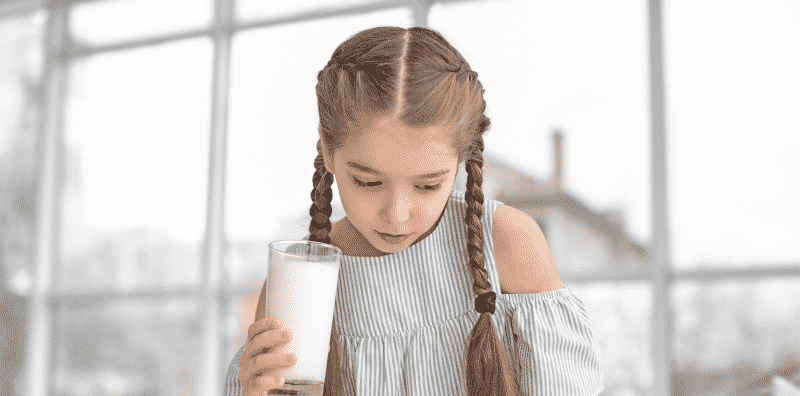
The increasing number of allergy cases is mainly in children making it the most common chronic condition in kids. Childhood allergies that most children normally resolve or ‘outgrow’ are starting to continue into adulthood, bringing yet another worry to burden parents.
but what exactly is an allergy?
A true allergy is a medical condition that results from your immune system inappropriately reacting to something harmless in our environment called an allergen (4). The immune response, called an allergic reaction, occurs because of this overshooting to something that doesn’t actually cause much of a threat. Like pollen in the case of hayfever, or to specific foods such as peanuts. The symptoms of an allergic reaction depend on where in your body it is occurring (for example, skin, lungs or digestive tract). Hay fever, for instance, affects the nose and eyes, while eczema affects the skin. They can range from mild (itchy mouth, a few hives) to severe (throat tightening, difficulty breathing). Other conditions such as asthma, which affects the lungs is closely related to an allergy but with slight differences to the underlying causes.
Food allergies affect the gut, skin, airways, lungs, and sometimes the entire body through the blood vessels. This can lead to anaphylaxis – a serious whole-body allergic reaction that is sudden in onset and can cause death. More than 170 foods have been reported to cause allergic reactions with eight major food allergens – milk, egg, peanut, tree nuts, wheat, soy, fish and crustacean shellfish – (responsible for most of the serious food allergy reactions) with an allergy to sesame becoming an emerging concern (5).
Whilst we have treatments for the symptoms of allergies, we do not yet have a cure or the ability to prevent them from developing in the first place.
and what isn’t an allergy?
It’s easy to confuse a food allergy with a much more common reaction known as food intolerance. While bothersome, and despite many shared unpleasant symptoms, food intolerance is a less serious condition that does not involve the immune system. Unlike a food allergy, intolerances generally occur because your body cannot properly break down food or the food irritates your digestive tract. Broadly categorised as physiological (e.g. lactose enzyme deficiency), functional (e.g. irritable bowel syndrome in response to FODMAPs) or pharmacological (e.g. sensitivity to food additives or components of foods, such as sulfites) (8). Intolerances can also be psychological (e.g. eating disorder) or in some cases without a defined cause (idiosyncratic) (6).
Allergic reactions to food can be life-threatening and require a strict exclusion of the offending food. Food intolerances, which can be unpleasant, do not pose the same threats. Complete exclusion might not be the best approach for food intolerances in the long term.
Unlike an allergy, a number of studies have found that having small amounts of offending foods with meals reduces the chances of experiencing symptoms of intolerance after consumption (7). Self-diagnosis of intolerances is extremely common, up to 20% of the UK population is estimated to have altered their diet to exclude foods based on a perceived ‘intolerance’. In fact Avoidant/Restrictive Food Intake Disorder (ARFID) is now a clinical condition reflecting the recognition of the growing number of people who exhibit food-avoidant and restrictive eating behaviours (8). It is important to speak with a healthcare professional before removing suspect foods from your diet. 34% of parents reported food allergies in their children but only 5% were found to have a true allergy (9). Implementing these unnecessarily restrictive diets are actually leading to malnutrition in kids (10). Avoiding certain foods in early life actually doesn’t pay off in preventing food allergies since early exposure is actually protective (11).
what you need to know
a food allergy is:
- an adverse response by your immune system
- usually comes on suddenly
- triggered by a small amount of food
- happens every time you eat the food regardless of how much or how frequently
- can be life-threatening
a food intolerance is:
- not mediated by your immune system
- usually comes on gradually
often relates to the amount of food - often relates to the frequency of eating the food
- is not life-threatening
about the author
Immunologist Dr. Jenna Macciochi unravels the science underlying strong immunity and teaches us how to be well in a modern world. Currently a lecturer at the University of Sussex, she specialises in understanding how nutrition, lifestyle, and gut health interact with the immune system in health and disease. Jenna is a Brighton (UK) based mum to twins, a perpetual kitchen experimenter with a passion for movement and exercise.
related articles
References
- Umasunthar, T., Leonardi-Bee, J., Hodes, M., Turner, P. J., Gore, C., Habibi, P., … Boyle, R. J. (2013). Incidence of fatal food anaphylaxis in people with food allergy: a systematic review and meta-analysis. Clinical and Experimental Allergy : Journal of the British Society for Allergy and Clinical Immunology, 43(12), 1333–1341.https://doi.org/10.1111/cea.12211
- Levy, M. L., Price, D., Zheng, X., Simpson, C., Hannaford, P., & Sheikh, A. (2004). Inadequacies in UK primary care allergy services: national survey of current provisions and perceptions of need. Clinical <html_ent Glyph=”@amp;” Ascii=”&”/> Experimental Allergy, 34(4), 518–519. https://doi.org/10.1111/j.1365-2222.2004.1945.x
- Gupta, R., Sheikh, A., Strachan, D. P., & Anderson, H. R. (2007, January). Time trends in allergic disorders in the UK. Thorax. https://doi.org/10.1136/thx.2004.038844
- Making Sense of Allergies: A guide to what allergies are (and aren’t) and the evidence for causes and treatments (2015). Sense About Sciencehttps://senseaboutscience.org/wp-content/uploads/2016/09/Making-Sense-of-Allergies-1.pdf
- ‘Guidelines for the diagnosis and management of food allergy in the United States: Report of the NIAID-sponsored expert panel’ (2010) Journal of Allergy and Clinical Immunology, 126(6 SUPPL.). doi: 10.1016/j.jaci.2010.10.007.
- Zopf, Y. et al. (2009) ‘The differential diagnosis of food intolerance.’, DeutschesArzteblatt international. Deutscher Arzte-Verlag GmbH, 106(21), pp. 359–69; quiz 369–70; 4 p following 370. doi: 10.3238/arztebl.2009.0359.
- Savaiano, D. A. et al. (2013) ‘Improving lactose digestion and symptoms of lactose intolerance with a novel galacto-oligosaccharide (RP-G28): A randomized, double-blind clinical trial’, Nutrition Journal. BioMed Central Ltd., 12(1). doi: 10.1186/1475-2891-12-160.
- Thomas, J. J. et al. (2017) ‘Avoidant/Restrictive Food Intake Disorder: a Three-Dimensional Model of Neurobiology with Implications for Etiology and Treatment’,Current Psychiatry Reports. Current Medicine Group LLC 1. doi: 10.1007/s11920-017-0795-5.
- Venter, C. et al. (2008) ‘Prevalence and cumulative incidence of food hypersensitivity in the first 3 years of life’, Allergy: European Journal of Allergy and Clinical Immunology, 63(3), pp. 354–359. doi: 10.1111/j.1398-9995.2007.01570.x.
- Isolauri, E. et al. (1998) ‘Elimination diet in cow’s milk allergy: Risk for impaired growth in young children’, The Journal of Pediatrics. Mosby, 132(6), pp. 1004–1009. doi: 10.1016/S0022-3476(98)70399-3.
- Du Toit, G. et al. (2015) ‘Randomized trial of peanut consumption in infants at risk for peanut allergy.’, The New England journal of medicine. NIH Public Access, 372(9), pp. 803–13. doi: 10.1056/NEJMoa1414850.