stress and the gut
Science has proven significant correlations between levels of stress and quality of life; more specifically in the context of gut health and gastrointestinal related disorders, which are suffered by 40% of us at any given time.
The Gut-Brain Axis
The ‘gut-brain axis’ describes a back-and-forth communication pathway between the central nervous system and the gastrointestinal tract, which uses signalling hormones and all sorts of other fancy messengers to manage what we do and how we feel on a daily basis.
A key player in this set up is our microbiome – the community of microorganisms, mostly bacteria, living in our gut- which directly impacts the messages being sent up and down our bodies.
There has been a huge amount of research into this gut-brain-microbiotic interaction in recent years, and findings suggest that both acute and chronic stress will change the balance in our microbiome by favouring unhelpful bacteria, which can result in feelings of anxiety and depression. Research has also shown that those with depression and anxiety have lower diversity of bacteria in their guts and that specific bacteria may also increase the risk of depression and anxiety.
Stress and the Body
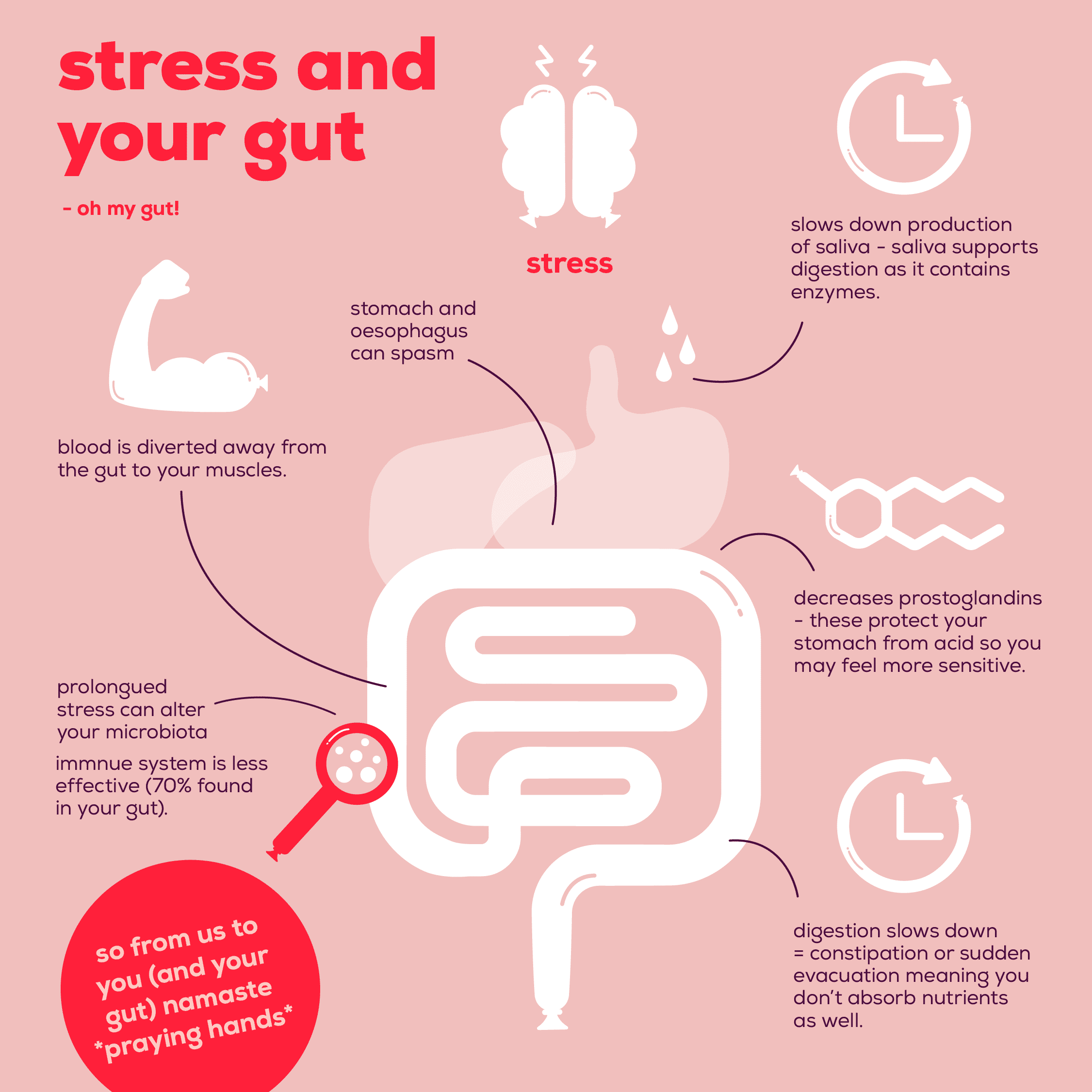
In response to stress (perceived or actual), our body produces the hormone cortisol. Cortisol has many important functions in the stress response but of relevance to the gut, it:
- Diverts blood away from the gut to your muscles (to fight or run from your stressor);
- It slows down the production of saliva in your mouth meaning the enzymes available to break down food is reduced (impairing digestion)
- Decreases prostaglandins, which protect your stomach from acid so you might have a more sensitive tummy when you are stressed;
- Slows down digestion or causes sudden evacuation (diarrhoea), which might mean you aren’t absorbing nutrients as well;
- Downregulates your immune system (70% is found in your gut); and
- It can cause the stomach and oesophagus to spasm.
All of this is fine in the short term, but where stress is prolonged and food isn’t digested properly, it can really play havoc on the delicate ecosystem found in your gut.
On the flip side, however, it has been proven that digestion happens more effectively when eating in a relaxed and calm state. Scientific studies have shown that a well-nourished and diverse microbiome will help to increase the production and communication of the ‘happy hormone’ serotonin, which is sent up to the brain to lift our spirits, calm us down and essentially help us live on the brighter side of life.
Tips
So with all that science out there, the question still begs; how does one manage that complicated cycle of feelings/food/work/general life without stressing about not being stressed….??! Phew. Well, it’s really not that hard. Queue our tips to help gut you going.
De-stress
What works for you will be different from someone else so focus on what helps you relax, whether a yoga class, a walk or even some mindfulness. Do something that helps you get away from the stress of daily life.
Try to be relaxed before eating
Don’t eat on the go, sit down without distractions (like your phone) and really focus on the food in front of you. When was the last time you took a deep breath to fill up your lungs? Try taking three deep breaths before you eat to promote a ‘rest and digest’ state.
Keep a diary to understand why you feel stressed
It could be working out too hard, not getting enough sleep, worrying about work or family. We are all unique but do what you can to get to know yourself better and work on how you manage that stress. We’ve got a Gut Diary that includes Gut Started pages, The Gut Stuff Stool Chart and space for your weekly shopping list. Get yours here.
Then once you’ve done all of that? Chill out and let your body do its thing; those little microbes are smarter than you think!
Interested in finding out more tips?
Read more tips and tricks on managing your stress & helping out your gut on our app. You can download it for free below.
References
De Palma, G., Collins, S. M., Bercik, P., & Verdu, E. F. (2014). The microbiota–gut–brain axis in gastrointestinal disorders: stressed bugs, stressed brain or both?. The Journal of physiology, 592(14), 2989-2997.
Moloney, R. D., Johnson, A. C., O’mahony, S. M., Dinan, T. G., Greenwood‐Van Meerveld, B., & Cryan, J. F. (2016). Stress and the microbiota–gut–brain axis in visceral pain: relevance to irritable bowel syndrome. CNS neuroscience & therapeutics, 22(2), 102-117.
Valles-Colomer, M., Falony, G., Darzi, Y. et al. The neuroactive potential of the human gut microbiota in quality of life and depression. Nat Microbiol 4, 623–632 (2019) doi:10.1038/s41564-018-0337-x
https://www.nhs.uk/live-well/eat-well/common-digestive-problems-and-how-to-treat-them/
MAYER, E. The neurobiology of stress and gastrointestinal disease
Gut 2000;47:861-869.
Yaribeygi H, Panahi Y, Sahraei H, Johnston TP, Sahebkar A. The impact of stress on body function: A review. EXCLI J. 2017;16:1057–1072. Published 2017 Jul 21. doi:10.17179/excli2017-480
