travel and the gut
Written by Bridgette Wilson
Whether it’s for a staycation or venturing further afield, taking a break from our normal routine and soaking up all those new sights, tastes and adventures can be very refreshing however, and we know this only too well, sometimes your gut can refuse to play ball turning those holiday dreams into a bit of a nightmare…
We got the lowdown from our pal Dr Bridgette Wilson on how travel can impact our gut and simple remedies to look after it while away, time to get packing!
Changes to the food you eat can wreak havoc on your gut…
If you normally eat a healthy high fibre diet at home but then on holiday you are on a white bread, cheese and meat diet you can find yourself seriously backed up – taking a packet of chia seeds on holiday with you and drinking a glass of soaked chia seeds each morning can help as well as finding a fresh fruit stall to grab some extra fibre there. Kiwi fruit contain an enzyme that may help the gut to move, stone fruit such as plums, peaches and nectarines help draw water into the gut creating a natural laxative effect to get you moving again.
Flying away on a jet plane?
Long-haul flights can lead to bloating and constipation due to the food, the dehydrating air conditioning and changes in pressure. Pack some high fibre snacks such as seed bars or oat cakes and take your own water supply so you don’t have to keep ringing the call bell for a tiny cup of water every 15 minutes to maintain your hydration.
So runny, it’s not funny.
Food poisoning on holiday is also very common. Changes in diet, stress and intake of contaminated food and beverages can all have an impact on your gut microbiome, which can open the door for invading pathogens.
One study demonstrated that taking prebiotics before and during travel to countries considered high risk for traveller’s diarrhoea, reduced the incidence of this happening. This may be due to increasing the number of friendly bifidobacteria in the gut, giving you a stronger gut population to help defend against invading pathogens. [1]
If you do get food poisoning you can take probiotics to help introduce more of the friendly gut bugs to help stabilise your gut population. You also may need to take antibiotics for some mor serious cases of food poisoning, if so start the probiotics after the antibiotics finish. A probiotic containing Saccharomyces boulardii CNCM I-745 may be protective against travellers diarrhoea. [2]
If you have diarrhoea, vomiting and/or a high temperature the risk of dehydration can be high, this is dangerous and can leave you feeling much worse than the food poisoning alone. Your wee is a good indicator of dehydration, if it is darker or even brown in colour you need to get some fluid back in fast. Rehydration salts help force water back into your body to rehydrate you quicker. Isotonic fluids (e.g. some sports drinks) work in the same way but aren’t as strong.
But it’s not all bad!
Getting away from everyday life often gives us the chance to prioritise relaxation which can go a long way in managing our stress levels. Your mental health hugely effects your gut health and vice versa (read more about the gut-brain axis here), and science now shows that learning how to manage stress or even reduce it where you can will go a long way in supporting your mental health and in turn, your gut.
Sleep! Ultimately, your gut needs a good old sleep as much as the rest of your body does so hit snooze and take advantage of that lie in.
Did you know that movement is one way of influencing the microbes that live within your gut for the better? One to consider while you’re clocking up all those steps on your city break (or running for a connecting flight!).
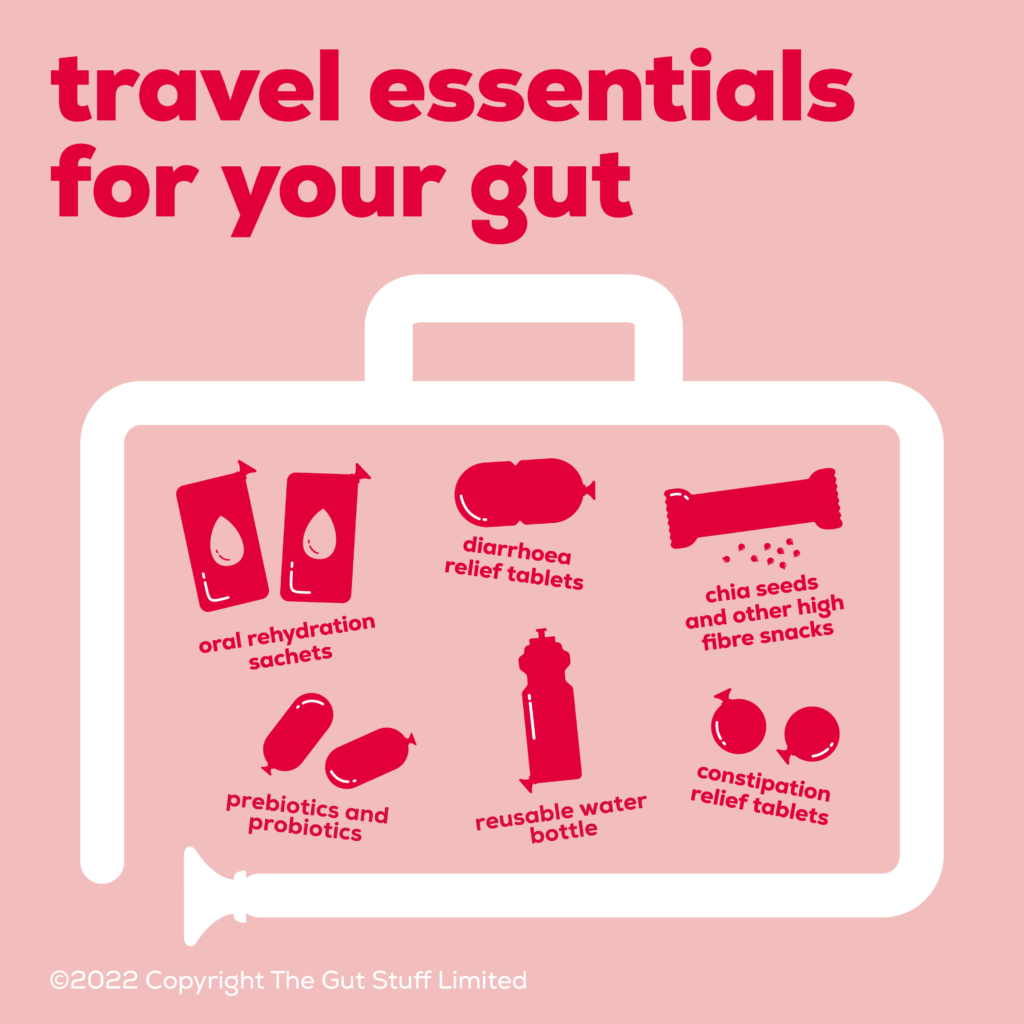
So what can you pack to care for your gut while travelling?
Here’s a super handy list to keep in mind while preparing for your upcoming travels:
References
- 1.Drakoularakou et al 2010 – https://www.nature.com/articles/ejcn2009120
- 2. McFarland and Goh 2019 – https://pubmed.ncbi.nlm.nih.gov/30278238/
About the author
Dr Bridgette Wilson is a gut specialist clinical and research dietitian with a wealth of clinical dietetic experience both in the NHS and private healthcare. Her award-winning PhD research on the Low FODMAP diet and Prebiotics in Irritable Bowel Syndrome (IBS) and Ulcerative Colitis, has given her a great depth of knowledge to help her patients attain good symptom control.